Need to Know
Who is at Risk for Skin Problems?
- Older adults - the skin is less elastic, thinner, and easily torn. An older adult has less fatty tissue or padding over bony parts of the body like the tailbone, shoulders, back of head, heels and hips.
- Persons with one or more medical problems such as diabetes, kidney disease, and heart disease that affect treatment and healing.
- Persons who cannot hold their urine or bowel movements, or have diarrhea. The urine and diarrheal stool are acidic and enzymes in stool digest the skin.
- Persons who do not eat a healthy diet. Good nutrition is needed for the skin to heal.
- Persons who have had a stroke, paralysis, or nerve changes lose sensation in areas of the skin preventing them from feeling excess pressure on the skin.
- Persons who have a loss of mobility, making it difficult to easily change position while in a bed or chair.
- Persons in pain who are not able or unwilling to move because of discomfort.
- Persons who have casts on a leg or arm or wear braces on the legs. Anything applied to the skin can cause repeated friction and pressure.
What are the Signs of a Skin Infection?
- Pain at the site of injury
- Redness and swelling
- The site will feel warm to the touch
- An open wound or cut might weep yellowish or greenish drainage
What is a Pressure Ulcer?
- A pressure ulcer is an injury to the skin due to unrelieved, prolonged pressure or a combination of pressure and friction.
- Constant pressure on an area of skin reduces blood supply to the area. Over time this causes the skin to break down and form an open sore or ulcer.
- If left untreated or allowed to progress, a pressure ulcer can easily become infected.
- The seriously ill and disabled person who is less mobile is most at risk.
- Pressure ulcers most often form on bony areas of the body where there is little cushion between bone and the skin. Most form on the lower part of the body such as the tailbone, lower spine, buttocks, hips, and heels. Other common areas are the back of the head, back of the ears, shoulders, elbows, ankles, and between the knees where the legs rub together.
Prevention is the Key. As a caregiver you can help prevent a person from getting a pressure ulcer. Regular skin care and keeping a close watch of a person’s skin are key. Once a pressure ulcer forms it can become a serious problem. There are 4 different stages or levels of severity of pressure ulcers.
Pressure Ulcer Stages

Stage I – Skin is not broken but is red or discolored. The redness or change in color does not fade within 30 minutes after moving or turning off of the pressure area. The skin may be painful.

Stage II – There is a break in the top layer of the skin, creating a shallow open sore. It may look like a scrape (abrasion), blister, or a shallow crater (ulcer) in the skin. Drainage may or may not be present. Usually the area is tender and painful.

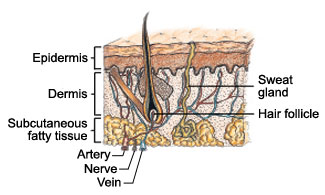
Stage III – The break in the skin extends through the epidermis (first skin layer) and dermis (second skin layer) into the fatty tissue. The wound is deeper than in Stage Two, but does not show tendon, muscle or bone.

Stage IV – The break in the skin and tissue extends into tendon and muscle and can go as far down as the bone. Usually dead tissue and drainage are present. In stages III and IV there may be little or no pain due to tissue damage.
What Causes Pressure Ulcers?
Anyone at risk for skin problems can develop a pressure ulcer.
- Pressure ulcers are caused by pressure on the skin, shear, friction, and moisture.
- Pressure -The more pressure and the longer time it is placed on the skin, the greater risk of injury. A person can have a small amount of pressure on the skin, but if it is not removed in a couple of hours, a pressure ulcer can form.
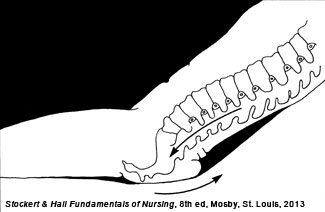
- Shearing force – When one layer of tissue slides over another, this causes the skin to separate away from deeper tissues and damage blood vessels. Shear commonly occurs from pulling on the body against resistance or friction from the surface of a bed. When a person lies in bed with the head raised over 30 degrees on several pillows, there is pressure on the tailbone. The skeleton slides down while the skin stays fixed, against the bed sheets. This causes shearing.
- Friction – Rubbing of the skin against a surface. When you move a person up in bed and their hips or heels drag against the sheet, this causes friction. Pulling a person up in bed the incorrect way can cause sheet burns.
- Moisture – Moisture left on the skin over several hours will soften and damage the skin. Moisture comes from excess sweating, urine, wound drainage or diarrhea on the skin.