Need to Know
How We Breathe
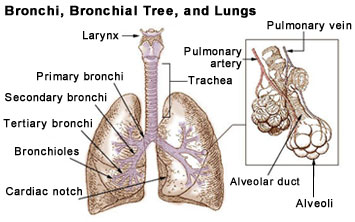
Normally when we inhale or breathe in, air moves in and out of our lungs freely and easily. As we breathe in, the oxygen in the air travels through very tiny airways in the lungs to small air sacs called alveoli. There, oxygen travels across the membranes of the alveoli to enter the blood by attaching to red blood cells. The cells circulate to deliver oxygen to all tissues of the body.
After the cells of the body use oxygen, carbon dioxide forms. This gas then travels through the circulation to the alveoli of the lungs. The carbon dioxide moves across the membranes of the alveoli into the small airways of the lungs, where the gas exits the body as we exhale or breathe out.
For each of us to live we must breathe in oxygen and breathe out carbon dioxide. The body regulates this very nicely, keeping normal levels of oxygen and carbon dioxide in the blood. Normally, we breathe without thinking.
The rate at which we breathe depends primarily by the amount of carbon dioxide circulating in our blood. When carbon dioxide levels rise, this causes us to breathe faster. When we breathe faster, more oxygen enters our lungs and we exhale or breathe out to remove the extra carbon dioxide.
The body protects itself if oxygen levels become too low. Low oxygen will cause a person to breathe faster and to inhale more oxygen through the lungs.
Breathing is automatic, but when we exercise hard, catch a bad cold, or simply want to take a nice deep breath, we will consciously breathe more often or more deeply to get more oxygen to our cells.
Who Needs Oxygen Therapy?
A person receives oxygen to prevent or treat hypoxemia, low blood oxygen. With hypoxemia there is not enough oxygen to meet the needs of the body’s tissues and cells.
In order to function properly, your body needs a constant level of oxygen circulating in the blood to cells and tissues. When this level of oxygen falls below a certain amount, hypoxemia occurs.
Various diseases cause hypoxemia, requiring the temporary or long term use of oxygen.
Acute Hypoxemia (from short-term oxygen use). Examples of conditions include, but are not limited to:
- Pneumonia – inflammation of the lungs from infection
- Bronchiolitis - viral infection of lower airways, common in infants
- Short term worsening of chronic obstructive lung disease
- Short term worsening of heart failure
Chronic Hypoxemia (from long-term oxygen use). Examples of conditions include, but are not limited to:
- Chronic obstructive lung disease (bronchitis, emphysema, asthma)
- Cystic fibrosis
- Bronchiectasis (born with condition) or Acquired Bronchietasis (Adult age)
- Widespread lung tumor
- Pulmonary hypertension
- Recurring congestive heart failure due to chronic cor pulmonale (right sided heart failure)
A doctor is able to determine if a person has hypoxemia by testing a blood sample taken from an artery. Another way is to use a pulse oximeter – a small device that clips on a finger. A pulse oximeter measures the oxygen saturation of your blood, which estimates blood oxygen levels.
Normal pulse oximeter readings range from 95 to 100 % in persons who do not have lung disease. Values under 90 % are considered low. A person who requires oxygen will learn what their normal oxygen saturation is. Oxygen therapy will be ordered to keep the person’s oxygen saturation at a healthy level.
Dangers of Oxygen Therapy
Oxygen Toxicity - Oxygen is a medicine that can cause serious effects if not given correctly. For some people, there is a delicate balance in how much oxygen they can receive. For example, persons with chronic obstructive lung disease (COLD) have limited airflow. This means that air gets trapped in the small alveoli (air sacs) of the lung as a result of mucous buildup or narrowing of the small airways.
When a person with COLD breathes in, the airways pull open to allow gas to flow past any obstruction. But, when the person exhales, the airways collapse and the air (including carbon dioxide) cannot get out.
When these diseases progress, a person holds more carbon dioxide in the blood than normal. Thus, the body is no longer able to sense small changes in carbon dioxide levels. A high level of carbon dioxide is no longer the trigger for breathing. In persons with COPD, small changes in oxygen become the trigger for breathing. So, if a person is given too high levels of oxygen, the stimulus to breathe disappears. In these individuals, giving too much oxygen can be deadly as a result of oxygen toxicity.
Oxygen Fire - Oxygen is a very combustible gas. It can cause other materials like grease, oil, bedding or clothes to ignite more easily and burn rapidly. A simple spark or static electricity can easily cause a fire if oxygen is nearby.
- Follow all precautions to be sure oxygen is stored and delivered in a well-ventilated area.
- Keep all oxygen equipment a minimum of 8 feet from any open flames.
- Do not use any electrical appliances that may cause sparks.
Oxygen Delivery
A person receives oxygen either by continous-flow or pulse-dose.
Traditional continuous-flow oxygen works the way the name suggests. It is delivered through a device as the patient breathes in and breathes out. It runs continuously.
In pulse-dosed flow, oxygen is delivered in a “dose” only as the patient breathes in. Pulse-dose technology allows oxygen delivery systems to save oxygen delivery. As a result, a person breathes in less total oxygen, without being at risk for hypoxia. This allows relatively small portable oxygen systems to be more efficient and last longer.
Oxygen Delivery Systems
Long term oxygen therapy is administered by one or a combination of three delivery systems: oxygen concentrator, compressed gas cylinder, or a liquid oxygen system. Each of the systems has unique advantages and disadvantages regarding operation, function, and cost.
A person’s choice depends on how much and when oxygen is needed and the level of daily activity. Cost or insurance restrictions may also affect choice. The person’s doctor, home health nurse, and home care provider of oxygen will select the system that best suits the person’s needs.
Oxygen Concentrators – A concentrator pulls air from a room and filters out other gases to provide only oxygen.
- Concentrators are the most common delivery system used and most economical.
- The system needs electricity and may increase a person’s home electric bill.
- An electrical generator or a backup compressed oxygen cylinder is needed in case of a power failure.
- Tell the electric company if the person for whom you provide care has an oxygen concentrator.
- Portable concentrators are available, each weighing about 10 pounds.
- This system is cost-effective for people requiring low-flow continuous oxygen and those with limited mobility.
Compressed Oxygen – Oxygen is stored as gas under high pressure in a cylinder or tank.

- Tanks can be large (stationary), medium (portable), or small (ambulatory).
- The cylinders are fitted with a flow meter and a regulator and are made of steel or aluminum.
- The aluminum cylinders are easier to manage because they weigh less than the steel tanks.
- Once a cylinder is empty, the home oxygen provider must refill the cylinder.
- Stationary tanks are quite large and only moved by the provider during delivery.
- Although portable tanks are easier to move, each weighs more than 10 pounds and is not designed to be carried. A portable tank usually lasts for about 5 hours.
- Ambulatory cylinders weigh less than 10 pounds and can be carried easily. An ambulatory tank delivers oxygen for at least 4 hours. People typically use this system for intermittent therapy, such as for exercise or during travel.
Liquid Oxygen – Oxygen is delivered by way of a liquid. Liquid oxygen turns into a gas when it is used. Large amounts of oxygen can be stored in a small container.
- A portable liquid oxygen system can be refilled from a larger liquid stationary system.
- A home oxygen provider usually refills a stationary system every 1 to 2 weeks depending on the amount used. This is often the system of choice for high volume users and active people.
Oxygen Conserving Devices
An Oxygen-conserving device (OCD) reduces the weight of portable oxygen containers. An OCD extends operating time on an oxygen system by not wasting oxygen through continuous flow. There are two common types of OCDs:
- Reservoir nasal cannula: Stores oxygen in a small chamber as a person exhales or breathes out. This oxygen is then used for delivery later when the person next inhales or breathes in.
- Demand pulsing oxygen delivery system: Delivers a burst of oxygen at the beginning of a breath. Oxygen does not flow out as the person exhales or breathes out, thus saving oxygen.
Oxygen Delivery Devices
Home oxygen therapy is usually given through a nasal cannula or a face mask. The person’s doctor will choose the best method to suit the person’s needs.

Nasal Cannula – The easiest, least expensive, most common, and most comfortable device for receiving oxygen.
A continuous-flow cannula is a plastic tubing that has two prongs or tips, each about ½ inch long that fit into each nostril of the nose. Place the prongs in the person’s nostrils and then slip the cannula around the person’s ears to make a lanyard under the person’s chin. The lanyard adjusts to a snug fit, keeping the prongs or tips in place. Oxygen flows through the cannula at a low flow rate with or without humidity.
A reservoir cannula works by storing oxygen in a small chamber as a person breathes out. When the person is ready to inhale, they get the stored oxygen. A person will be able to use a lower oxygen flow setting (compared with a continuous-flow) while still receiving the same amount of oxygen.

Oxygen Masks – There are several types of masks, each delivers a different concentration (percentage) of oxygen with or without humidity.
Simple face mask – delivers oxygen for short term therapy. It fits loosely around the face and delivers oxygen usually in a higher concentration than a nasal cannula.
Face mask with reservoir (rebreather or non-rebreather) – delivers higher concentrations of oxygen. The bag must be inflated to deliver the higher oxygen percentage. (A non-rebreather looks similar to a rebreather mask, but it has a special valve which prevents air from going back in to the bag during inhaling or exhaling).

Venturi mask– Delivers a more accurate concentration of oxygen than a re-breathing mask. The venturi mask is cone shaped and has special ports at the base of the mask to adjust higher concentrations of oxygen.
Oxygen Through Tracheostomy – A person who has an artificial opening in their neck into the trachea (tracheostomy) receives oxygen through a tracheostomy collar or a T-Tube.
T-Tube Tube – a T-shaped device that connects an oxygen tubing to the tracheostomy. It is used more commonly if a person is on a home ventilator.
Tracheostomy collar – A curved device with an adjustable strap that fits around a person’s neck and over the tracheostomy opening. The collar has two ports, an exhalation port that must remain open at all times and the port that connects to the oxygen container.
Transtracheal oxygen – oxygen flows through a thin tube inserted through the neck into the trachea (windpipe). A person is able to talk with the tube in place.